Neck Injury Lawyer in Wisconsin

Wisconsin Neck Injury Attorney
Whiplash
is by far the most common injury following Wisconsin Car Accidents.
Whiplash
is also quite common in the majority of all other Wisconsin Personal Injury Accidents. The reason for this is really quite simple, the neck and head are usually the most susceptible parts of the body whenever there is a large amount of force exerted on the human body. The relatively narrow neck (or cervical spine) supports the relatively large head. In a Whiplash Injury, the neck acts as a whip, causing the head to be forced back and forth. Whiplash often results in Neck Injury, but oftentimes Whiplash also results in a serious brain injury. Headaches
are very common following Whiplash.
Wisconsin Neck Injury Attorney
While we have offices in Milwaukee and Madison, we handle neck injury cases that happen throughout Wisconsin.
While Whiplash
is technically a non-medical term. Whiplash Neck Injuries
are also known by many other medical and non-medical terms:
- Neck Strain
- Neck Sprain
- Cervical Strain
- Cervical Sprain
- Flexion-Extension Injury
- Cervical Hyperextension Injury
- Acceleration-Deceleration Injury
- Soft-Tissue Injury
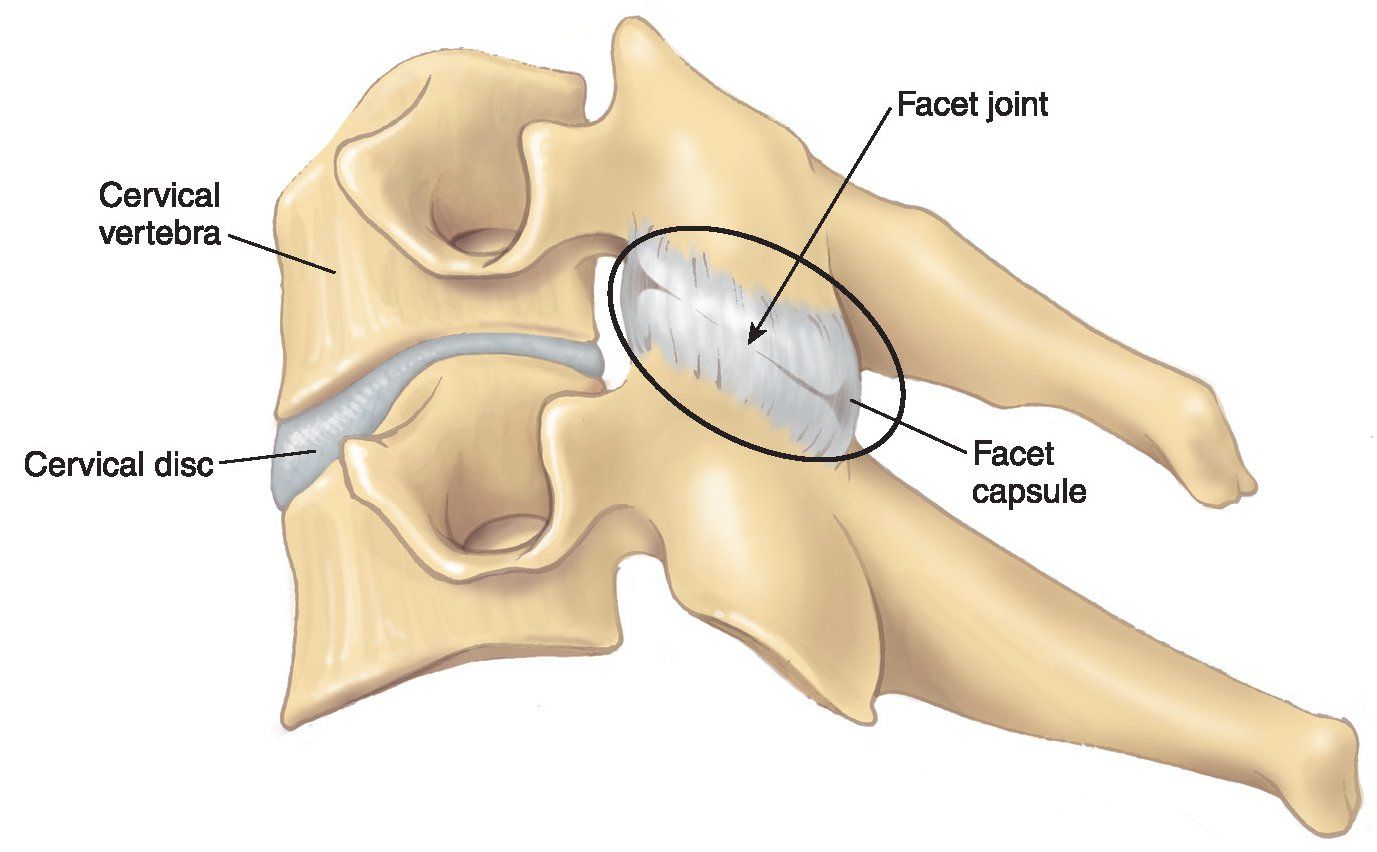
Neck Anatomy
Whiplash
can refer to an injury to any of the following:
- Cervical Vertebrae – the bones that make up the spinal column
- Cervical Disc – the rounded structure in between the Cervical Vertebrae
- Muscle – soft-tissue within the body responsible for movement
- Ligament – a band of fibrous tissue connecting one bone to another
- Tendon – a band of fibrous tissue connecting muscle to bone
- Joint – the point where two or more bones come together, allowing movement
The Neck or Cervical Spine
consists of 7 Cervical Vertebrae, labeled C1 through C7. Each Cervical Vertebrae
is separated and cushioned by a rubbery substance known as a Cervical Disc, the center of which is made of a gel-like substance. Muscles, Ligaments, Tendons and Joints
are all intertwined within the neck.
If the particular injury to the neck involves the muscles and tendons, then physical therapy, message, and/or chiropractic treatment may be recommended. If the symptoms do not improve with these types of treatments, then the injury may involve something more serious.
Cervical Facet Joint Injury
It is thought that over 60% of persistent neck pain is likely due to Facet Joint Injury. The Facet Joints
are also known as the Zygapophysieal or Apophyseal Joints. The Facet Joints
allow movement of the spine and, at the same time, provide support to the spine. The Facet Joints
allow you to bend forward, backward and side-to-side. Trauma to the Cervical Spine
can result in damage to the Facet Joints. The Facet Joints
are the point where the cervical vertebrae come together. In the Cervical Spine, there are two sets of Facet Joints on the side of each vertebrae (as opposed to the back of the spinal column in the thoracic and lumbar spine). The Cervical Facet Joints
are similar in size to the size of the joints between each bone in your fingers. The are two nerve endings within each of the Cervical Facet Joints.
These three factors make it clear why Facet Joint Injury
is the most likely cause of neck pain in most Whiplash Injuries:
- The location of the Facet Joints on the side of the vertebrae vs. the rear;
- The relatively small size of the Cervical Facet Joints; and
- The numerous nerve endings within the Cervical Facet Joints
Cervical Facet Joint Pain
can be localized to the cervical spinal column area, but it can also radiate into the shoulders and arms.
Diagnosis of Cervical Facet Joint Pain
Diagnosing Cervical Facet Joint
Pain is often difficult because the pain, at least in the acute phase, may mimic Cervical Disc Herniation. While a CT Scan may be helpful, it is unlikely to show most Cervical Facet Joint
injuries. The most definitive diagnostic tool is the Facet Nerve Block.
Facet Nerve Block
Proper Facet Nerve Block
testing is able to objectively identify those patients who have chronic facet pain by doing blinded testing on two different days. On the first day, two Facet Nerves are injected with an anesthetic. Since a single Facet Joint
is innervated by two nerves, elimination of the pain with that procedure can only be explained by the pain arising from the joint innervated by those two nerves (e.g., elimination of pain from the C5-6 Facet Joint by anesthetizing the C5 and C6 Facet Nerves). The problem is that after one test, the physician still cannot reasonably conclude whether they eliminated the pain or whether the patient just believes the pain has been eliminated.
Therefore, the patient must be brought back on a different day and informed that the physician is going to do the same thing again, but not necessarily on the same nerves and with an anesthetic that has a shorter or longer duration of action.
If C5 and C6 Facet Nerves
are again blocked, it should eliminate the pain again. If the nerves at another level are injected, such as C4 and C7, there should be no pain relief. If the nerves at C6 and C7 are blocked, it should eliminate half the pain. After the injections, the patient should be asked whether there was any change in their pain, the location of the change, if any, and how great a change in their pain occurred, if it occurred. If the patient can tell whether the pain was eliminated in total, not at all, or if a part of their pain changed, then their statement is objective evidence that can be tested against what the physician knows he or she did and what the patient reported on the initial testing. For example, if the nerves were blocked at C6 and C7, the physician then does another set of nerves (either C5 or C4) that either eliminates the rest of their pain or does nothing.
The patient is also asked which testing day resulted in longer lasting relief.
The likelihood that the patient just guessed the expected relief provided by the first two nerve blocks on the second day is one in three, the three possible answers being complete relief, no relief or partial relief. The likelihood that the patient just properly guessed whether the third nerve block eliminated the remaining pain or not is one in two. The likelihood that the patient just guessed which day had the longer lasting anesthetic is one in two. The likelihood that the patient guessed all three answers correctly is 1/3 x 1/2 x 1/2, which is 1/12th. Therefore, there is a 8 1/3% chance of guessing all three correctly. This means that the likelihood of the patient was not guessing is 91 2/3%. This is a very high probability rate in the field of medicine.
Treatment of Cervical Facet Joint Pain
Treatment of Cervical Facet Joint Pain can involve a number of different types of treatment. However, if the physician has properly administered the Cervical Facet Joint Nerve Blocks the physician is likely to recommend Radiofrequency Neurotomy of the Facet Joint Nerves.
Radiofrequency Neurotomy
Radiofrequency Neurotomy
is a minimally invasive surgical procedure involving the use of low level electrical stimulation to locate the exact Facet Nerve
causing pain and then severing that particular Facet Nerve. The nerve that is severed will eventually regenerate and the procedure may need to be repeated every 12-18 months. After second or third time, the procedure will likely not need to be repeated again. Many patients obtain relief and do not need any further procedures.
Cervical Disc Herniation or Rupture
Cervical Disc Herniation
refers to a compromise of one of the cervical discs located in between each cervical vertebrae. This Herniation
may come into contact or otherwise aggravate a nerve within the neck. When this occurs, the patient will likely have pain which may radiate into the arms. This is known medically as Radicular Pain. Patients with Cervical Disc Herniation
may suffer from pain that feels like an electrical shock into the arms. The patient may also have, tingling, numbness and muscle weakness into the arms. When this occurs, the nerves that run into the arms through the neck are being aggravated by the herniated disc.
Diagnosis of Cervical Disc Herniation or Rupture
The primary objective diagnostic tool for diagnosis of Cervical Disc Herniation
is the MRI, show in the photograph to the right. MRI
stands for Magnetic Resonance Imaging. MRI
essentially allows us to see 2 or 3 dimensional images of the soft-tissues within the human body. In a Cervical MRI, the radiologist uses the MRI to scan the Cervical Discs in order to look for any irregularities. MRI is quite accurate in the diagnosis of Cervical Disc Herniation.
As with most things in medicine, there are drawbacks to the MRI. The primary negative is that some people are claustrophobic and they have a difficult time with small, enclosed places and must be sedated in order to actually stay still long enough to complete the entire scan. The machine is also very loud. The machine makes a loud continuous pounding noise, almost like a hammer. Finally, some individuals are unable to have an MRI
due to heart conditions or metal instrumentation within their body. Overall, the benefits far outweigh the negatives of an MRI.
Treatment of Cervical Disc Herniation or Rupture
There are two types of treatment for Cervical Disc Herniations; Conservative or Surgical. The type of treatment is determined by the nature and severity of the pain and the ability of the patient to function.
Conservative Treatment of Cervical Disc Herniation or Rupture
Conservative treatment can consist of medication, physical therapy, traction, nerve blocks, or immobilization. Many patients with Cervical Disc Herniations
improve with conservative treatment and never need surgery.
Surgical Treatment of Cervical Disc Herniation or Rupture
If the patient does not recover adequately following conservative treatment, then surgery may be recommended. Surgical options can include the following:
- Anterior Cervical Discectomy and Spinal Fusion – This is the most common surgical procedure for Cervical Disc Herniation. Anterior Cervical Discectomy and Spinal Fusion involves the removal of the disc and then fusing the vertebrae together. Oftentimes a metal plate is added for stability.
- Anterior Cervical Discectomy without Spinal Fusion – This is the same procedure as above, however, the vertebrae are not fused toegether.
- Posterior Cervical Discectomy – This is less common for Cervical Herniations because the surgery occurs from the back of the patient, while the disc is in the front of the body.
- Posterior Cervical Decompression – This involves shaving and shaping the herniation or bulge in the disc.
- Posterior Cervical Laminaplasty – This procedure involves removing a portion of the bone, the lamina, to allow for more room for the spinal cord and nerve roots.
- Posterior Cervical Foraminotomy – This procedure involves removing small pieces of bone around the foramen, allowing for more room for the nerves without pressure.
If you or a loved one suffer from a Whiplash Neck Injury
due to the negligence of another, be sure to contact an experienced Wisconsin Personal Injury Attorney.